49 year female with fever
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through a series of inputs from the available global online community of experts intending to solve those patients' clinical problems with collective current best evidence-based inputs.
Fever since 15 days.
Abdominal discomfort since 15 days.
Generalized weakness since 15 days.
Decreased appetite since 15 days.
HOPI:
A 49 year female presented to the OPD with complaints of high grade Intermittent fever associated with chills, malaise and decreased appetite. Fever was relieved on taking medication. History of abdominal discomfort as tightness since 15 days not associated with vomiting. History of nausea associated with decreased appetite. No history of headache, retro orbital pain, cold, cough, chest pain, SOB, PND, Orthopnea, burning micturition.
she sought for consultation at local RMP and took medication (Antipyretic and Antibiotic), fever was releived upon taking medication associated with excessive sweating. She got fever spike on the same day, she sought for consultation at local hospital; she was treated with IV Antipyretic, Antibiotic and Analgesic medication daily on opd basis for 4 days. She stayed at home for the rest of 10 days and received treatment with Oral and IV Antipyretics, Antibiotics. Now admitted for further evaluation and management.
PAST ILLNESS:
No Comorbidities.
SURGICAL HISTORY:
S/P - Tubectomy under LA in 1997.
S/P - Hysterectomy with B/L salpingo-oophorectomy under GA in 2014 i/v/o massive Uterine fibroid.
PERSONAL HISTORY:
Moderately built and nourished.
Sleep decreased.
Appetite lost.
Bowel and bladder are regular.
No addictions.
GENERAL EXAMINATION:
Patient was conscious and coherent.
No pallor, Icterus, cyanosis clubbing,edema.
Cervical lymphadenopathy+
Neck rigidity.
Tonsillar enlargement with tonsilloliths and local pus.
Febrile.
VITALS:
PR: 92bpm; BP:110/80mmHg; RR: 22; SpO2: 98%@RA; Temp: 101°F; GRBS: 121mg/dl.
CVS: S1,S2+, No added sounds;
R/S: BAE+, Clear;
P/A: Soft, Upper abdominal tenderness, BS+;
CNS: HMF intact; GCS 15/15; B/L Upper and lower limb time and power are normal; Kernig's and Brudzinski sign -ve.
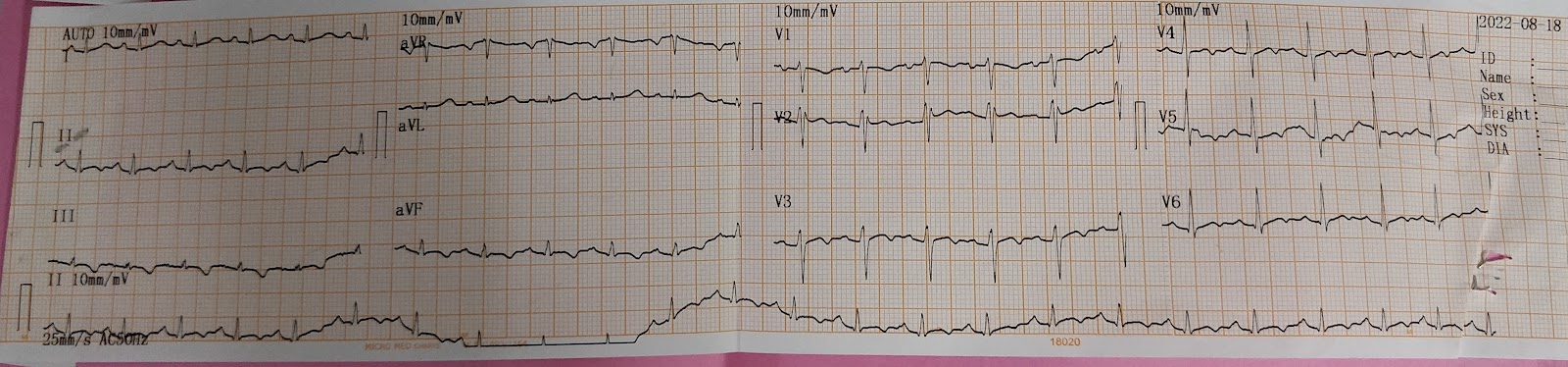
ECG AT PRESENTATION:
Day 1:-
Day 2:-
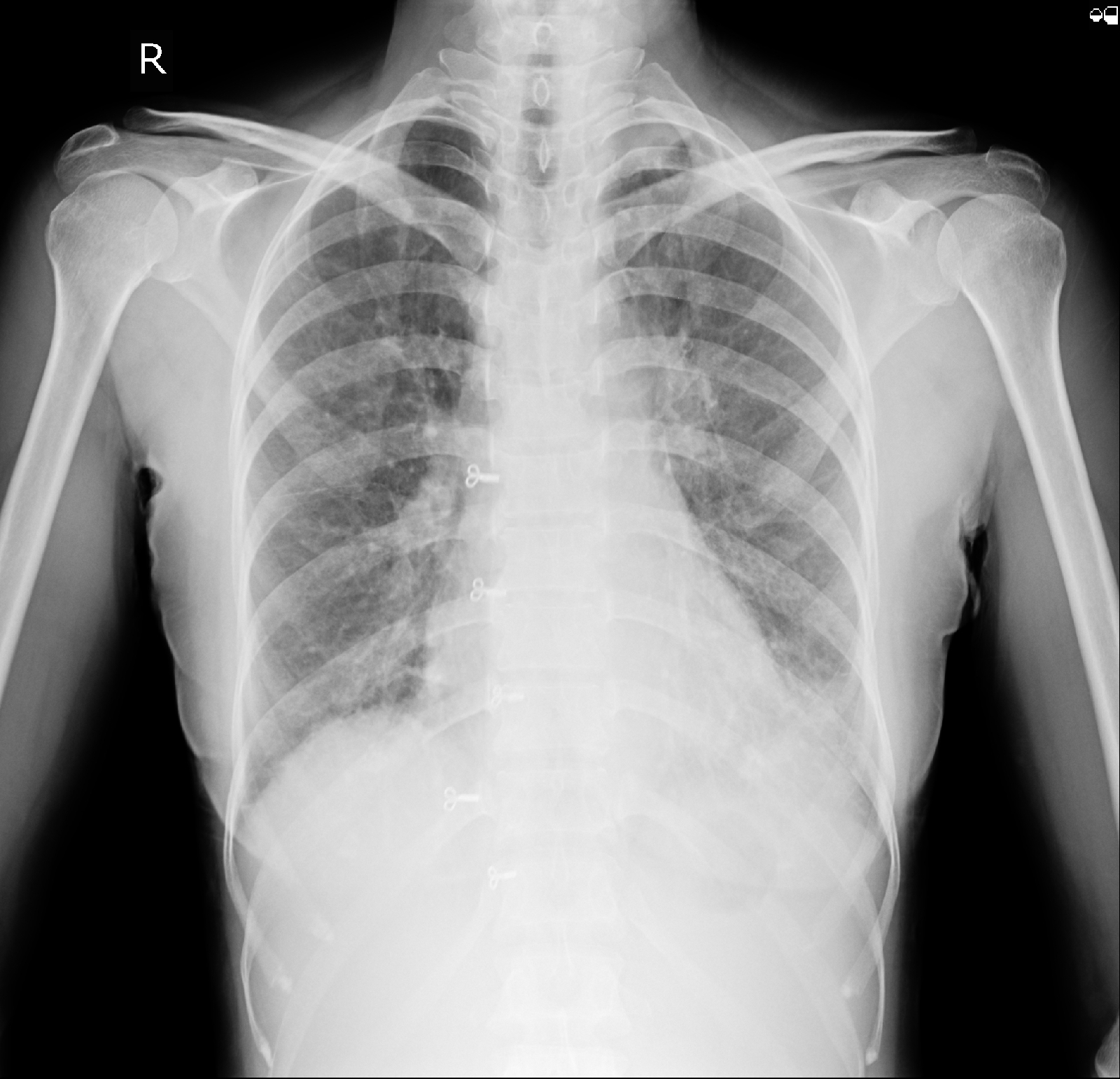
CHEST XRAY:
FEVER CHART:
INVESTIGATIONS CHART:
USG ABDOMEN:
On 18/08/2022
A 49 year female presented to the OPD with above mentioned complaints. Upon examination initial workup was done and ENT cross consultation was done I/v/o Enlarged tonsills and orders followed; throat swab was sent for Culture and sensitivity. Blood and urine culture were negative after 7 days of aerobic incubation which were sent on 17/08/2022. She was started on IV fluids, Cefriaxone antibiotic and other supportive management during the course in hospital. Her HB was 10.2, she was started on Oral Iron suppliments. USG ABDOMEN was done on 18/08/2022 which showed findings :
1. Liver of normal size and echotexture with normal PV, CBD and contracted gall Bladder.
2. Spleen of 13.8 cms with normal size and echotexture.
3. Rt kidney : 10.1×2.9 cms; Lt kidney : 10.5×3.5 cms; Normal size and echotexture with Corticomedullary differentiation maintained and Normal PCS.
4. Mild Spleenomegaly.
5. Post Hysterectomy.
2D ECHO was done on 19/08/2022 which showed e/o :
Mild TR; Trivial AR; No MR; No RWMA; No AS/MS; Sclerotic AV; Good LV Systolic function; Diastolic dysfunction; No PAH; IVC 0.7cms and collapsing; Minimal Pericardial effusion; RVSP 40mmHg.
Her fever spike was gradually subsided and general weakness improved. Upon examination Rt IAA and ISA region. Repeat USG was done which showed :
1. Liver of normal size and echotexture with PV 11mm and normal CBD.
2. Spleen of 11.2 cms with normal echotexture
3. Rt kidney
TREATMENT:
1. IVF NS/RL @75ml/hr.
2. INJ. NEOMOL 100ml / IV / SOS ( IF TEMP >=102°F)
3. INJ. CEFTIAXOME 1GRAM /IV /BD.
5. TAB. DOLO 650mg/ PO / TID
6. VITAL MONITORING.